
Diabetes is one of the most common lifestyle conditions worldwide, yet many people remain unsure about how to manage it day to day. Managing diabetes well is not only about taking medicines. It involves a structured care plan, healthy eating, physical activity, regular monitoring, and support from a trusted doctor or diabetic centre.
This guide explains the most important aspects of diabetes care in 2025. We will cover what a good diabetes care plan looks like, how remission is possible for some people, what to eat if you have diabetes, when medicines are needed, and how to safely manage sudden changes in blood sugar.
What Good Diabetes Care Looks Like
If you are searching for the best diabetes doctor or the most reliable diabetic centre near me, it is important to know what high quality care should include. Good diabetes care is never only about writing prescriptions. It is about helping you stay healthy for the long term by addressing every part of your health.
A good diabetes care plan should cover:

- Routine monitoring. This includes fasting and post-meal sugar levels, HbA1c every 3 to 6 months, cholesterol, kidney function, and urine albumin. These tests help detect problems early and track your progress.
- Screening for complications. Every year you should have an eye examination for retinopathy and a foot check to look for nerve or circulation problems.
- Nutrition and activity support. You should receive practical guidance on what to eat, how much to eat, and how to stay active. A plan that includes structured exercise is more effective than general advice.
- Access to technology. Tools such as continuous glucose monitoring (CGM) can help you understand how meals, activity, and stress affect your sugar levels. These insights often lead to better control.
- Written care goals. You should leave your consultation with clear instructions about what to do, when to follow up, and what results to aim for.
The best diabetes doctors focus on prevention, early detection, and personalised care. They also encourage lifestyle changes that improve your health span, not just your blood sugar numbers.
A Seven Day Framework for Diabetes Care
Managing diabetes requires consistency. A simple weekly structure can make it easier to stay on track.
Daily routine
- Check fasting blood sugar in the morning if advised.
- Include 10 to 15 minutes of gentle movement such as stretching or walking soon after waking.
- Eat a balanced breakfast that combines complex carbohydrates, protein, and fibre.
- Aim for 30 to 45 minutes of moderate activity such as brisk walking, cycling, or swimming along with muscle strengthening exercises at least thrice a week.
- If your doctor has recommended post-meal checks, measure your sugar levels 1.5 -2 hours after the main meal.
- Practice good sleep hygiene and aim for 7 to 8 hours of rest.
Weekly structure
- Include three strength sessions, which may be body weight exercises or gym-based training. Building muscle improves insulin sensitivity.
- Schedule one activity session that challenges your endurance, such as interval walking, cycling, or a VO₂ max test under supervision.
- Review your progress every week by tracking weight, waist circumference, and active minutes.
A SMART goal example is to reduce fasting glucose by 10 to 15 mg/dL in six weeks by improving diet and activity while losing 4 to 5 percent of body weight.
Is Diabetes Reversal Possible??
Many people now search for answers about diabetes reversal. Research shows that for some individuals, particularly those with early type 2 diabetes, remission is achievable.
The DiRECT trial from the United Kingdom demonstrated that an intensive weight management program, which began with a calorie restriction phase followed by structured support, helped nearly half of participants achieve remission. The key factor was sustained weight loss, which reduces fat stored in the liver and pancreas. Lowering this fat allows insulin-producing cells to recover and function better.
The chances of remission are highest within the first five to six years after diagnosis and in people who are not yet dependent on insulin. Even for those who do not reach remission, weight loss and lifestyle changes significantly reduce complications and the need for medications.
It is important to remember that remission is not a cure. Ongoing monitoring is still essential. Stopping medicines suddenly without medical supervision can be dangerous. The best approach is to work with a doctor or centre that runs structured remission programs and provides close follow up.
Creating an Effective Diabetes Diet Plan
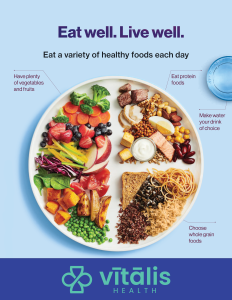
An effective diabetes diet plan does not mean that you cut out all the foods that you like. Diet is central to every diabetes mellitus care plan. But balance is the key. Make sure that each plate that you have is balanced in terms of macronutrients like carbohydrates, proteins and fats.
Foods to include
- Whole grains such as brown rice, oats, and millets.
- Legumes and pulses such as chana, rajma, and moong dal.
- Lean protein from fish, chicken, eggs, and pulses.
- Fibre rich vegetables and fruits, focusing on non-starchy options.
- Nuts and seeds in small portions.
Foods to limit
- Refined carbohydrates like white bread and sweets.
- Sugary beverages and fruit juices.
- Fried foods and processed snacks.
- Excess saturated fats.
Sample meal plan
- First Bite: Start your day with a low glycemic index food like soaked almonds.
- Breakfast: Oats or millets cooked with dal or pulses, topped with nuts and chia seeds and sliced apple.
- Mid morning: Buttermilk or hummus with cucumber.
- Lunch: Red rice with bran, dal or legume curry, grilled fish or chicken, and a large vegetable salad and a bowl of curd.
- Snack: Roasted chana or a small fruit with peanut butter. Green Tea.
- Dinner: Ragi dosa / Roti with sambar / Dal and sautéed spinach.
The diet should be tailored to individual needs. Portion sizes, carbohydrate distribution, and cultural preferences all matter. The best diabetes doctors and centres help personalise meal plans rather than giving one size fits all advice.
Medications and Their Role
Medicines are important tools in type 2 diabetes care. They help lower blood sugar while lifestyle measures take effect.
- Metformin is the most common first line medicine. It improves the way the body uses insulin and reduces glucose production in the liver.
- Sulfonylureas such as glimepiride stimulate the pancreas to release insulin. They are effective but can cause low blood sugar if meals are missed.
- DPP 4 inhibitors, SGLT2 inhibitors, and GLP 1 receptor agonists are newer options. Some of these also protect the heart and kidneys.
The choice of medicine depends on age, weight, kidney function, and other health conditions. Medicines should only be started, changed, or stopped under medical guidance.
Understanding Blood Sugar Numbers
Knowing your sugar numbers helps you make sense of test results.
- A normal fasting sugar level is between 70 and 99 mg/dL.
- Prediabetes is defined as a fasting sugar between 100 and 125 mg/dL.
- Diabetes is diagnosed when fasting sugar is 126 mg/dL or higher on two separate occasions.
- HbA1c shows your average sugar over 3 months. A result of 6.5 percent or higher confirms diabetes.
- For most adults with diabetes, the goal is to keep HbA1c below 7 percent, although this target may vary based on individual factors.
How to Quickly Lower Blood Sugar Safely
Many people search for what to drink to lower blood sugar immediately. The truth is that there is no magic drink that can safely bring high sugar down instantly.
- If sugar levels are high, the safest steps are to drink water, remain physically active if there are no warning symptoms, and seek medical advice if levels are persistently above 240 mg/dL. Severe hyper-glycemia with symptoms requires urgent medical care.
- If sugar levels are too low, which means below 70 mg/dL, use the 15 15 rule. Take 15 grams of fast acting carbohydrate such as glucose tablets, half a cup of juice, or a spoon of sugar. Wait 15 minutes and recheck. Repeat until levels are above 70 mg/dL. Severe hypoglycemia is a medical emergency.
The Vitalis Health Approach
At Vitalis Health, diabetes care is guided by longevity medicine principles. We combine traditional medical expertise with fitness based assessments and structured lifestyle programs.
Our services include VO₂ max testing, body composition analysis, and grip strength measurement to personalise exercise prescriptions. We use CGM in the early phase to help patients see how food and activity affect their glucose. Our digital tools support ongoing monitoring and self management.
For patients searching for the best diabetes doctor or a reliable diabetic centre near me, our focus is on safe, personalised, and proactive care. Our Reboot Diabetes program follows the strongest evidence on remission, pairing structured nutrition with coaching and measurable progress.
Final Takeaway
Good diabetes care is not only about medicines. It is about structured plans, healthy diets, and regular monitoring. The right approach can reduce complications, improve quality of life, and even achieve remission for some patients.
Working with the right doctor or centre helps you stay on track. If you or someone you know is living with diabetes, now is the best time to start a care plan that looks beyond sugar numbers and focuses on long term health.
